Revised: January 3, 2013
Accepted: January 23, 2013
Published online: February 23, 2013
Cold is a seasonal and circadian risk factor for cardio- and cerebrovascular morbidity and mortality. Colder temperatures have been associated with higher blood pressure (BP), based on studies which show that BP levels measured during the summer months are generally lower than those measured during the winter months. Residents in geographic areas which have greater seasonal temperature differences show greater fluctuation in BP. Surprisingly, atmospheric pressure, rainfall, and humidity were not related to BP levels. The increased sympathetic nervous activity due to cold, as evidenced by elevated BP and by plasma and urinary catecholamines, has been proposed as being the underlying etiology. Patients with heart failure may experience, in cold conditions, endothelial dysfunction and produce fewer endogenous vasodilators (e.g., nitric oxide, prostaglandins) and more endogenous vasoconstrictors (e.g., endothelin), thus increasing afterload. Arterial stiffness is also related to seasonal BP changes. Increased BP, arterial stiffness and endothelial dysfunction could predispose to increased coronary and cerebrovascular events. Improved protection against lower temperatures or increased doses of existing medications or the addition of newer medications could lead to a reduction in increased cardiovascular mortality in winter. Here, we briefly review findings from existing literature and provide an update on seasonal long-term variation in BP along with the related complications.
- Citation: Charach G, Shochat M, Argov O, Weintraub M, Charach L, Rabinovich A, Ayzenberg O, George J. Seasonal changes in blood pressure: Cardiac and cerebrovascular morbidity and mortality. World J Hypertens 2013; 3(1): 1-8
- URL: https://www.wjgnet.com/2220-3168/full/v3/i1/1.htm
- DOI: https://dx.doi.org/10.5494/wjh.v3.i1.1
According to some studies, lower temperatures in the winter are associated with mortality, with more deaths occurring in the winter than in the summer and most of them being due to cardiovascular and cerebrovascular events related to blood pressure (BP) changes among the elderly[1,2]. A seasonal impact on arterial BP has been demonstrated in several studies on hypertensive and normotensive patients of all ages[3-7]. There is a tendency for both systolic BP (SBP) and diastolic BP (DBP) to rise in the winter[3-13]. The larger population studies have shown mean winter-summer differences of 4-9 mmHg for SBP and of 0.6-5 mmHg for DBP[3,14]. While seasonal variation of BP affects all age groups, greater fluctuations were seen among the hypertensive elderly[10-12]. The seasonal differences in BP that we had found in elderly populations were much higher (18% variability)[10] than those reported in other studies on normotensive and hypertensive populations of all ages in the United States, United Kingdom, Italy, Holland, Japan, Iraq, Israel and Russia[3,8,10,15-20].
Thomas et al[21] reported that measurements of an elevated BP may vary by 40%, depending on the time of day and month of year. The magnitude of seasonal BP differences is controversial. Stout et al[16] studied normotensive elderly in their own homes or in residential homes and found seasonal temperature differences to be very low and statistically non-significant. In contrast, Kent et al[13] found significant associations between outdoor temperature and BP levels which remained after adjustment for various confounders, including season, and argued that outdoor temperature had the main impact and not the season itself. However, in other studies where BP was measured in the same temperature conditions, the main influence was season and not outdoor temperatures[13].
Several studies have evaluated the direct association between meteorological factors (temperature, humidity, atmospheric pressure) and circadian BP variability. Morning BPs and pre-waking morning BP surges on the coldest day were significantly higher than those on the warmest day (pre-waking morning SBP surge of 20.8 ± 1.3 mmHg vs 15.3 ± 1.3 mmHg, respectively, P = 0.0004). The magnitude of nocturnal BP decline on the coldest day was significantly greater than that on the warmest day (15.8% ± 0.7% vs 13.9% ± 0.7%, respectively, P = 0.01)[22]. According to those authors, outdoor temperature is an important determinant of morning BP, pre-waking morning BP surge and the magnitude of nocturnal BP decline. They concluded that these findings may have important implications in the management of hypertension and prevention of cardiovascular events[22,23].
The aim of this review was to summarize our findings from an earlier study[10] and to provide data that have since accumulated on seasonal long-term variation in BP and its related complications.
Clinical human and animal models have shown clear-cut BP responses to temperature changes[13-24]. Outdoor temperatures may have differing effects on autonomic and cardiovascular systems. Antihypertensive therapy has been found to modify autonomic responses and the resulting autonomic tone, which potentially affects the presumed increase in peripheral vasomotor tone related to the colder temperatures in the winter[25]. Previous studies indicated that outdoor temperature may have stronger effects on females, due to their choice of garments or to biological differences[12,24]. Older populations may be more susceptible to the effects of outdoor temperature on BP since many cardiovascular risk factors, such as arterial stiffening, worsen with age[10-13].
SBP and DBP showed significant univariate relationships with the season (more than with temperatures)[3-12]. All other covariates [age, gender, race, region, population density, education, income, community poverty, smoking status, alcohol use, body mass index (BMI), diabetes, and current hypertensive medication status], with the exception of dyslipidemia, may be significantly related to SBP and a given season. DBP was also significantly related to the season and to all the other covariates, with the exception of alcohol use and diabetes status. Several parameters other than BP, such as, pulse, glucose, low-density lipoprotein (LDL) cholesterol levels and others vary seasonally as well[13,26].
Several studies reported on the novel finding that the time of year, characterized by season, is secondary in importance to the outdoor temperature’s association with BP[13]. The suggested etiology was that cold increases sympathetic nervous activity, as evidenced by elevated BP measurements and plasma and urinary catecholamine (noradrenaline) concentrations[25,27]. Niimi et al[27] looked into whether factors pertaining to seasonal variations exist in humans as responses of the sympathetic nervous system to the gravity-dependent BP regulation and reported that muscle sympathetic nerve activity (MSNA) has an essential role in BP regulation in humans. The lower BP in warm temperatures has been attributed to cutaneous vasodilatation, loss of water and increased sodium excretion due to sweating[15,28]. These factors have been implicated as potential mechanisms by which BP increases in cold conditions. The seasonal variation of BP in patients with chronic kidney disease seemed to have no correlation with the stage of the disease or change in body weight, but it was inversely associated with outdoor temperatures. These results suggested that volume status might not be a key mechanism for causing seasonal variation in BP[29].
Vascular wall rigidity also influences BP. Arterial stiffness is related to the BP changes between summer and winter. Pulse wave velocity (PWV), a widely used clinical indicator of arterial stiffness, was correlated with winter-summer differences in SBP (r = 0.272, P = 0.012), but not with DBP (r = 0.188, P = 0.085). Age was strongly correlated with PWV (P < 0.001)[30]. Human and animal studies have demonstrated physiological mechanisms for this response and identified factors relevant to sympathetic nervous system activation, such as isoprenaline-induced relaxation of aortae and the renin-angiotensin system (stiffness)[31,32].
Wave intensity analysis (WIA) is another modality that measures effects of sympathetic excitation and elevation of BP on mechanical (rigidity-elasticity) properties of the common carotid and femoral arteries. The diameters and arterial stiffness parameters of the right common carotid artery and the right common femoral artery in healthy young men were measured by WIA at baseline and during cold pressor testing and found to be correlated with cold[32].
BP is a product of cardiac output as well as peripheral resistance and heart rate (HR). Cardiac output and stroke volume in normotensives significantly decreased by 10% and 15% from summer to winter, respectively, (P < 0.05) whereas HR and systemic vascular resistance decreased by 5% and 11%, respectively (P < 0.05). Norepinephrine (NE), plasma renin activity (PRA), and plasma aldosterone (PA) participate in mediating hemodynamic changes[33]. PA increased by 59% from summer to winter (P < 0.05), whereas, plasma NE (PNE) plasma epinephrine and PRA increased by 19%, 2%, and 17%, respectively (P = NS for each). Across the four seasons, mean arterial pressure significantly correlated with PRA and PA (P < 0.05 and P < 0.05, respectively), whereas systemic vascular resistance significantly correlated with PNE and PRA (P < 0.05 and P < 0.05, respectively). Dramatic counter-regulatory hemodynamic and hormonal adaptations are involved in maintaining a relatively constant BP[33]. Plasma NE levels are increased, largely reflecting sympathetic nerve stimulation insofar as plasma epinephrine levels are not increased. Unfavorable effects include vasoconstriction with increased vascular resistance, myocardial damage, and reduced renal blood circulation[11,13,33].
In cold conditions, neurohumoral responses help increase heart function and maintain BP and organ perfusion, but chronic activation of these responses is detrimental to the normal balance between myocardial-stimulating and vasoconstricting hormones and between myocardial-relaxing and vasodilating hormones[3,11,13,24-26,33-37]. The heart contains many neurohumoral receptors (α1, β1, β2, β3, angiotensin II type 1 and type 2, muscarinic, endothelin, serotonin, adenosine, cytokine), but the role of these receptors is not yet fully defined. In patients with heart failure, β1 receptors (which constitute 70% of all cardiac β receptors) are down-regulated, probably in response to intense sympathetic activation. The result of down-regulation is impaired myocyte contractility and increased HR.
Hormonal changes are known to have more chronic effects than neural sympathetic changes. The data on seasonal hormonal regulation are controversial. Radke et al[33] reported that anti-diuretic hormone (ADH) is released in response to a fall in BP (in the summer) via various neurohormonal stimuli. Increased ADH decreases renal excretion of free water, possibly contributing to hypervolemia and hyponatremia. Atrial natriuretic peptide is released in response to increased atrial volume and pressure, while brain (B-type) natriuretic peptide is released from the ventricle in response to ventricular stretching[33]. In contrast, Hirvonen et al[34] showed insignificant changes in catecholamines. While mean plasma noradrenaline concentrations diminished significantly from autumn to spring, and even more in the winter-summer group, there was no statistically significant difference between the groups. Adrenaline levels also showed a trend to decrease, and that change became significant when calculated by using the combined means of both groups. Plasma homovanillic acid and β-endorphin values were on the same level in all seasonal samples in both groups. By the spring, plasma serotonin levels decreased by about 50% in both groups. Hirvonen et al[34] showed a correlation with BP and anxiety in the autumn (r = 0.367), while endorphins and hysteria had a negative correlation in the winter (r = 0.370) and 5-hydroxy indole acetic acid and obsession had a positive correlation in the spring (r = 0.351).
Seasonal changes in HR and BP and FiO2 were shown to be associated with autonomic nervous system control. In the winter, the HR is higher and the oxygen consumption is lower, although training can increase vagal control and lower the HR and BP[35].
It has been posited that other seasonal variables, such as sunlight, may have an effect on BP. However, a number of studies have shown that atmospheric pressure (which can be used as a proxy for sunny weather), rainfall, and humidity were not related to BP[36-40]. Other factors that vary with the time of year, such as exercise, stress levels (e.g., summer holidays), mood (bipolar disorders), cognitive function, various health behaviors and biological processes, have all been shown to influence BP[29,35,41]. Other risk factors of hypertension and stroke, such as BMI (weight gain), are higher in the winter months. One study reported that the mean increase in SBP/DBP in the winter was significantly higher in underweight individuals than in individuals who were normal/overweight/obese (P < 0.05)[42]. Levels of inflammatory biomarkers (e.g., CRP and ICAM-1) are also associated with colder outdoor temperatures[43-45]. BP, preprandial glucose, A1C, and LDL cholesterol varied seasonally in patients with diabetes, with higher values in the winter and lower values in the summer[26].
The prevalence of orthostatic hypotension is higher in the summer[36-45]. Animal studies have shown that various amines (serotonin tyramine, phenylethylamine isoamylamine and others) are found in the plasma of ponies, and that concentrations increase significantly in the spring in comparison to winter in order to compensate for the vasodilatation (decreased vascular resistance) at higher temperatures[46]. The sympathetic nervous system plays an important role in thermoregulation as well as in BP regulation, and the process is related to orthostatism. Arterial smooth MSNA has an essential role in BP regulation in humans[11,13,46].
During the summertime, peripheral vascular resistance is reduced partly because of inhibition of the baroreflex response due to skin vasodilatation[11,13]. Heat stress reduces the sensitivity of the spontaneous baroreflex control of HR during orthostasis, but not during supine rest[11]. Central blood volume decreases with increasing skin blood flow, and the sensitivity of the integrative baroreflex control of total peripheral vascular resistance is reduced in heat-stressed humans. The altered baroreflex responsiveness in HR and peripheral vasomotor control as well as central hypovolemia are related to orthostatic intolerance in hot environments[36]. Volume status related to heat might be a main mechanism in causing orthostatic hypotension[47].
There is evidence that BP differs between geographical areas[18]. Colder climates are associated with higher BPs, and residents in regions with greater seasonal temperature differences show greater BP fluctuations[9,24]. Our earlier study on a large elderly population with hypertension living in a subtropical East Mediterranean region showed an 18% seasonal variation in BP[10]. Different racial and ethnic groups react differently to temperature changes, suggesting the possibility that temperature is a contributor to the higher cardiovascular mortality observed in African-Americans compared to Caucasians[13,30,48]. The groups with fewer years of education or low income may be more exposed to outdoor temperatures since they are more likely to have poorer indoor temperature control and may have careers which require more time outdoors[10,11]. Race, stroke-risk region, education, anti-hypertensive medication use, and age did not show any modification effect on any of the relationships between same-day temperatures and BP (P > 0.05)[13]. Several studies have raised the question of whether environmental stresses have differing effects on black populations compared to non-blacks, although there was no evidence of any difference[30-48]. Gender was shown to modify the relationship between temperature and BP in some studies[11,23] but not in others[13].
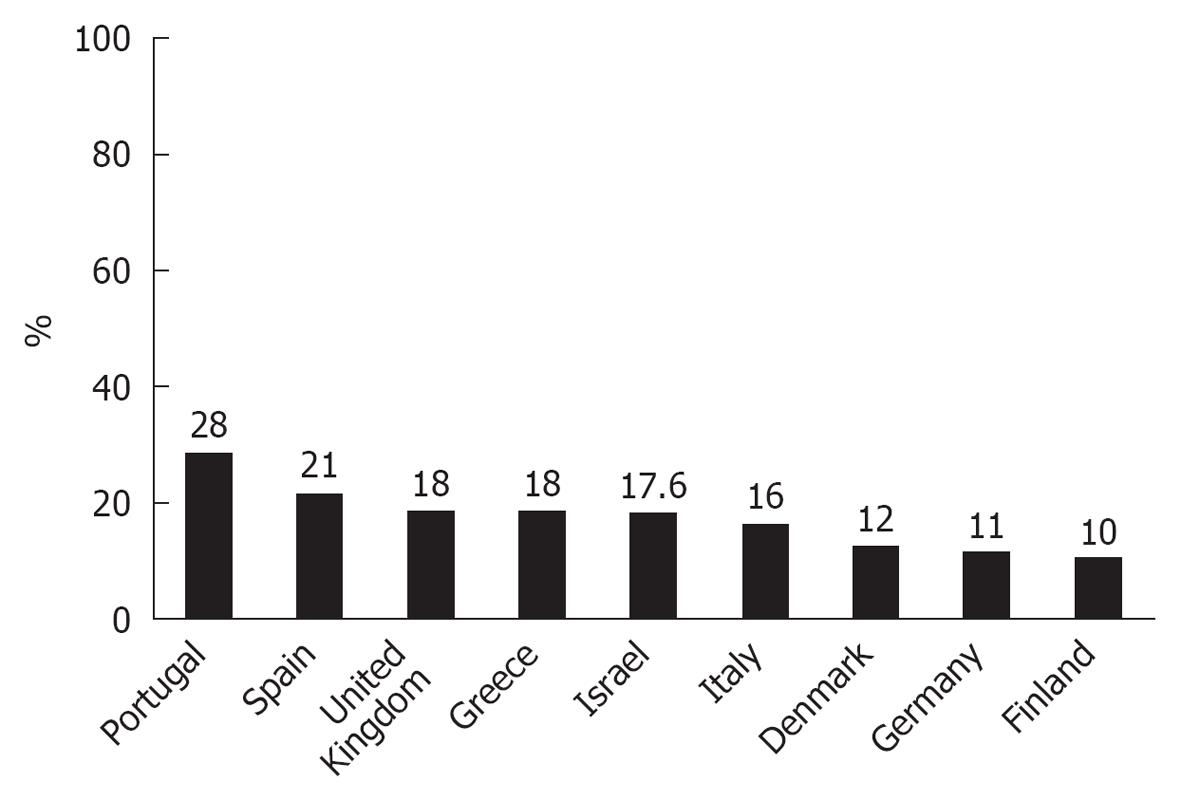
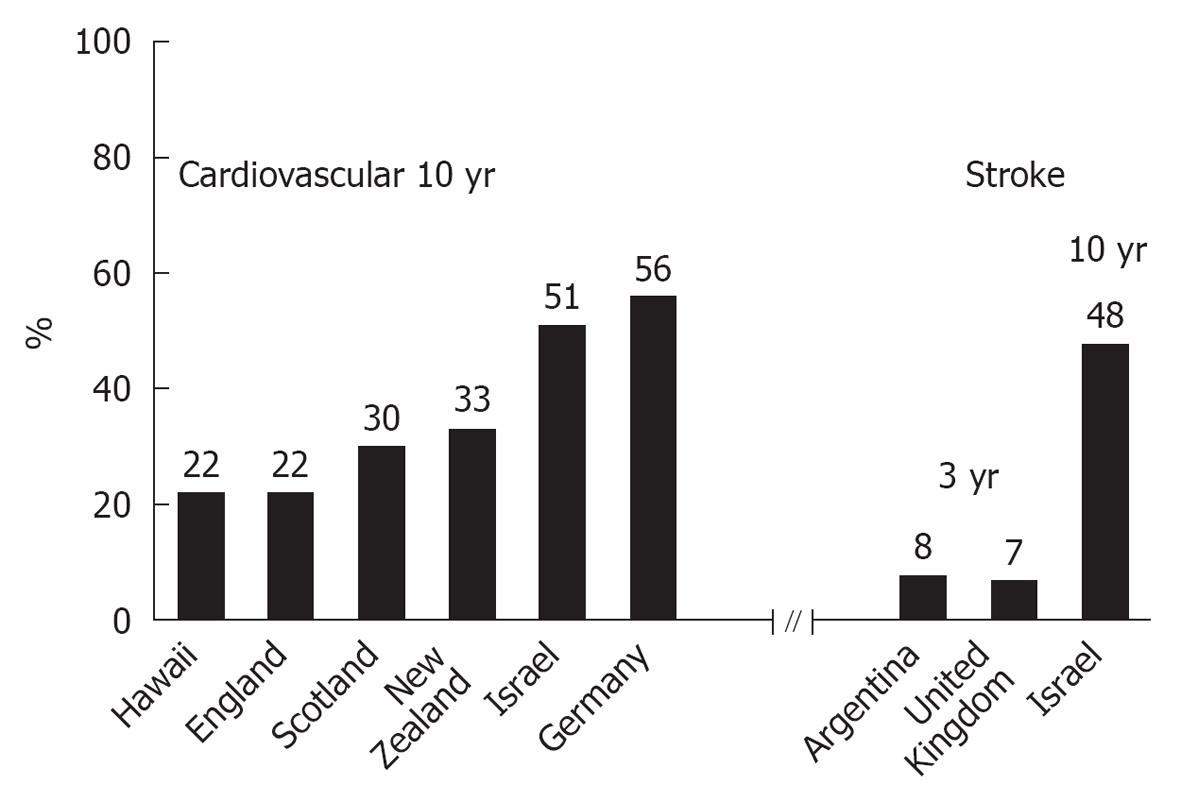
Many studies showed increased all-cause and cardiac mortalities in the winter compared to the other seasons (Figures 1 and 2)[1,11,13,49-67]. Cold weather generally showed a delayed health effect up to several weeks. The same trend was observed even in the most developed societies[1,52-60]. Healy’s analysis of data from 1988 to 1997 indicated that a relative excess of winter mortality was highest in southern Europe, Ireland, and the United Kingdom, where seasonality in mortality was estimated as being between 18%-28%[53]. He also noted that the Scandinavian and other northern European countries were relatively unaffected by the problem[53]. The cold-stressed heart and other organs produce tumor necrosis factor α (TNFα)[44]. This cytokine increases catabolism and is possibly responsible for cardiac dysfunction, which may accompany severely symptomatic HF as well as other detrimental changes. The failing heart also undergoes metabolic changes with increased free fatty acid utilization and decreased glucose utilization. These changes may become therapeutic targets[13,33]. Harmful effects include vasoconstriction with decreased preload and after-load, direct myocardial damage (including apoptosis), reduced coronary and renal blood flow, and activation of other neurohumoral systems (including ADH system)[11,13,33]. Patients with HF and cold-induced stress have endothelial dysfunction. They produce fewer endogenous vasodilators (e.g., nitric oxide, prostaglandins) and more endogenous vasoconstrictors (e.g., endothelin), thus increasing afterload, all of which factors predispose to coronary and cerebrovascular events.
Measurements of maximal oxygen intake and muscle strength commonly show parallel seasonal changes. However, potential effects upon body mass and body fat that increase in the winter may be counteracted by changes in food intake[14]. In developed societies, body fat commonly increases during the winter, with parallel changes in blood lipids, BP and blood coagulation - changes that are not always fully reversed during the following summer[11,13,52,61-66,68-72]. Health consequences of seasonal variations in physical activity, including an increased vulnerability to cardiac catastrophe and a year-by-year increase in total body fat, seem most likely to occur if the average level of physical activity for the year is low[14].
Exposure to decreased temperature is associated with an increase in the inflammation marker levels of CRP, soluble VCAM-1 and soluble ICAM-1 among elderly men, suggesting that inflammation markers are part of intermediate processes, which may lead to cold-related but not to heat-related cardiovascular deaths[44]. Other inflammatory markers, such as the white blood cell count, TNFα, interleukins-1β, -6 and -8, were not associated with cold and cardiovascular mortality[44].
Many studies report a seasonal pattern to stroke (Figure 2), which has a strong relationship with BP[2,48,51,55-61,67,70-72]. Stroke-prone rats have been found to have exaggerated BP responses to cold exposure[49]. Tienviboon et al[50] proposed that cold windy winter weather was the predisposing factor for the attack of reversible cerebral vasoconstriction syndrome (RCVS). RCVS has reversible multifocal narrowing of the cerebral arteries, as demonstrated on magnetic resonance angiography studies, in addition to brain edema and infarcts[50]. The consistent effect across various human demographic groups suggests that this is a real physiological phenomenon and not an artifact of living conditions[50].
Cardiovascular disease and stroke disproportionately affect the elderly[2,51,54-60,67]. Considering the graying of societies worldwide, it is becoming more and more imperative to expend considerable energy in an effort to prevent these complications in the first place and to treat them as promptly and effectively as possible when they are diagnosed.
Seasonal changes have implications in physical activity for fitness and human health[14]. Photosensitivity and nutrient shortages mediate animal hibernation via the hypothalamus and changes in leptin and ghrelin concentrations. Opportunities for hunting and crop cultivation determine seasonal activity in underdeveloped human societies, but temperature and rainfall are dominant factors in developed societies, usually over-riding innate rhythms. Both questionnaire data and objective measurements show that many groups of all ages increase their physical activity from winter to spring or summer. For example, the prevalence of being overweight, sedentary behavior and age were found to be inter-related among shift workers[14]. Most developed societies show increased all-cause mortality, including cardiac mortalities, in the winter[10,11,13,52-54,61-66,68-70]. Health consequences of seasonal variations in physical activity, including an increased vulnerability to cardiac catastrophe and a year-by-year increase in total body fat, seem most likely if the average level of physical activity for the year is low. Public health recommendations should emphasize the importance of maintaining physical activity during adverse environmental conditions by adapting clothing, modifying behavior and exploiting any available air-conditioned indoor facilities[14,52]. Improved protection against cold temperatures could lead to a reduction in the winter excess of cardiovascular mortality[12,24,53-57]. It has been postulated that people who are habitually involved in physical activity are better able to tolerate the cold stresses and are generally healthier than those who do not exercise[24]. BP and plasma catecholamine and serotonin levels decrease while practicing winter physical activities[14,24]. People who are involved in winter sports develop physiological adaptations: changes in their humoral status (e.g., decreased levels of serotonin) and enhanced vagal control either suggest adaptation or reflect seasonal variation from autumn to spring and show less significant seasonal BP changes[35]. Although it is generally advantageous for older people to be physically active in order to prevent circulatory disease, there may be a rationale for advising that that they should avoid intense activity at certain times of the day, especially in the winter[52]. Not uncommonly, patients need to increase the dose of antihypertensive medications or add another group of antihypertensive medicines during the winter months[10].
Many studies report a seasonal pattern to stroke, which is strongly related to BP[43]. The risk for stroke and transient ischemic attack increases exponentially with age, and BP is a potent modifiable target for reducing the risk for stroke in the elderly. In elderly patients with isolated systolic hypertension and in those with intracranial atherosclerotic disease, the lowering of BP has consistently been shown to be well tolerated and effective in reducing the risk for stroke and its complications. Evidence suggests that ambulatory BP monitoring may provide a more sensitive means of detecting patients at risk as well as for monitoring the therapeutic effect. The association of BP with season and outdoor temperature was examined in the Three-City Study, a population-based longitudinal study on 8801 subjects who were 65 years of age or older[11]. Outdoor temperature and BP were strongly correlated, especially in patients who were 80 or older. It was suggested that careful monitoring of BP and antihypertensive treatment during periods of extreme temperatures could contribute to reducing the consequences of BP variations and their complications in the elderly[24]. Preferable medications are agents that modify the renin-angiotensin system, particularly angiotensin receptor blockers, while calcium channel blockers may confer additional benefit in stroke protection alongside BP lowering[11,13,52,56,57].
In most of the reviewed studies, the patients were examined under indoor conditions, which are similar in winter and summer due to the use of air conditioning. However, patients generally live and function in different environments. Most of the cited studies lack data on outdoor and out-office BP where conditions may be different than in the doctor’s office. In addition, the selected reports do not deal with the “white coat” effect and “masked hypertension”. The former is a phenomenon where patients exhibit elevated BP in a clinical setting or the doctor’s office but not in other settings and is believed to be due to the anxiety some people experience at those venues. The latter is the opposite, with BP being elevated during daily activities but not in the office or clinical setting.
Seasonal changes in BP call for special attention with regard to both primary and secondary prevention. While satisfactory control of hypertension can be easily achieved during warm seasons, extra care must be exercised during cold seasons in terms of close monitoring aimed at prompt response to any shift of BP levels from desirable limits. This is exceedingly important in patients with previous cardiovascular events or predisposing factors for advanced atherosclerosis. Moreover, during cold periods, individuals at substantial risk for cardiovascular attacks should be considered for more intensive BP-lowering treatment, either by using more potent agents or by increasing the doses of their regular medications.
Esther Eshkol, the institutional medical and scientific copyeditor, is thanked for editorial assistance.
P-Reviewers Protogerou AD, Alok G, Toru M S- Editor Jiang L L- Editor Hughes D E- Editor Zheng XM
| 1. | Stewart S, McIntyre K, Capewell S, McMurray JJ. Heart failure in a cold climate. Seasonal variation in heart failure-related morbidity and mortality. J Am Coll Cardiol. 2002;39:760-766. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 141] [Cited by in F6Publishing: 147] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 2. | Feigin VL, Anderson CS, Anderson NE, Broad JB, Pledger MJ, Bonita R. Is there a temporal pattern in the occurrence of subarachnoid hemorrhage in the southern hemisphere Pooled data from 3 large, population-based incidence studies in Australasia, 1981 to 1997. Stroke. 2001;32:613-619. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 42] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Brennan PJ, Greenberg G, Miall WE, Thompson SG. Seasonal variation in arterial blood pressure. Br Med J (Clin Res Ed). 1982;285:919-923. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 366] [Cited by in F6Publishing: 362] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 4. | Khaw KT, Barrett-Connor E, Suarez L. Seasonal and secular variation in blood pressure in man. J Cardiac Rehabil. 1984;4:440-444. [Cited in This Article: ] |
| 5. | Näyhä S. Adjustment of blood pressure data by season. Scand J Prim Health Care. 1985;3:99-105. [PubMed] [Cited in This Article: ] |
| 6. | de Swiet M, Fayers PM, Shinebourne EA. Blood pressure in four and five-year-old children: the effects of environment and other factors in it’s measurement--the Brompton study. J Hypertens. 1984;2:501-505. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 26] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Jenner DA, English DR, Vandongen R, Beilin LJ, Armstrong BK, Dunbar D. Environmental temperature and blood pressure in 9-year-old Australian children. J Hypertens. 1987;5:683-686. [PubMed] [Cited in This Article: ] |
| 8. | Woodhouse PR, Khaw KT, Plummer M. Seasonal variation of blood pressure and its relationship to ambient temperature in an elderly population. J Hypertens. 1993;11:1267-1274. [PubMed] [Cited in This Article: ] |
| 9. | Al-Tamer YY, Al-Hayali JM, Al-Ramadhan EA. Seasonality of hypertension. J Clin Hypertens (Greenwich). 2008;10:125-129. [PubMed] [Cited in This Article: ] |
| 10. | Charach G, Rabinovich PD, Weintraub M. Seasonal changes in blood pressure and frequency of related complications in elderly Israeli patients with essential hypertension. Gerontology. 2004;50:315-321. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 48] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Alpérovitch A, Lacombe JM, Hanon O, Dartigues JF, Ritchie K, Ducimetière P, Tzourio C. Relationship between blood pressure and outdoor temperature in a large sample of elderly individuals: the Three-City study. Arch Intern Med. 2009;169:75-80. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 170] [Cited by in F6Publishing: 186] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 12. | Barnett AG, Sans S, Salomaa V, Kuulasmaa K, Dobson AJ. The effect of temperature on systolic blood pressure. Blood Press Monit. 2007;12:195-203. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 128] [Cited by in F6Publishing: 140] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 13. | Kent ST, Howard G, Crosson WL, Prineas RJ, McClure LA. The association of remotely-sensed outdoor temperature with blood pressure levels in REGARDS: a cross-sectional study of a large, national cohort of African-American and white participants. Environ Health. 2011;10:7. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 14. | Shephard RJ, Aoyagi Y. Seasonal variations in physical activity and implications for human health. Eur J Appl Physiol. 2009;107:251-271. [PubMed] [Cited in This Article: ] |
| 15. | Giaconi S, Ghione S, Palombo C, Genovesi-Ebert A, Marabotti C, Fommei E, Donato L. Seasonal influences on blood pressure in high normal to mild hypertensive range. Hypertension. 1989;14:22-27. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 57] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Stout RW, Crawford V. Seasonal variations in fibrinogen concentrations among elderly people. Lancet. 1991;338:9-13. [PubMed] [Cited in This Article: ] |
| 17. | Brueren MM, Schouten BJ, Schouten HJ, van Weel C, de Leeuw PW, van Ree JW. No relevant seasonal influences on office and ambulatory blood pressure: data from a study in borderline hypertensive primary care patients. Am J Hypertens. 1998;11:602-605. [PubMed] [Cited in This Article: ] |
| 18. | Abdulla K, Taka M. Climatic effects on blood pressure in normotensive and hypertensive subjects. Postgrad Med J. 1988;64:23-26. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Tanaka S, Konno A, Hashimoto A, Hayase A, Takagi Y, Kondo S, Nakamura Y, Iimura O. The influence of cold temperatures on the progression of hypertension: an epidemiological study. J Hypertens Suppl. 1989;7:S49-S51. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 20. | Gapon LI, Shurkevich NP, Mikhaĭlova IM, Gubin DG. [Circadian rhythms and seasonally dependent variability of arterial pressure in patients with arterial hypertension in the Khanty-Mansiysky region]. Klin Med (Mosk). 2004;82:22-25. [PubMed] [Cited in This Article: ] |
| 21. | Thomas C, Wood GC, Langer RD, Stewart WF. Elevated blood pressure in primary care varies in relation to circadian and seasonal changes. J Hum Hypertens. 2008;22:755-760. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Murakami S, Otsuka K, Kono T, Soyama A, Umeda T, Yamamoto N, Morita H, Yamanaka G, Kitaura Y. Impact of outdoor temperature on prewaking morning surge and nocturnal decline in blood pressure in a Japanese population. Hypertens Res. 2011;34:70-73. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 23. | Takenaka T, Kojima E, Sueyoshi K, Sato T, Uchida K, Arai J, Hoshi H, Kato N, Takane H, Suzuki H. Seasonal variations of daily changes in blood pressure among hypertensive patients with end-stage renal diseases. Clin Exp Hypertens. 2010;32:227-233. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 24. | Kimura T, Senda S, Masugata H, Yamagami A, Okuyama H, Kohno T, Hirao T, Fukunaga M, Okada H, Goda F. Seasonal blood pressure variation and its relationship to environmental temperature in healthy elderly Japanese studied by home measurements. Clin Exp Hypertens. 2010;32:8-12. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 25. | Fu Q, Zhang R, Witkowski S, Arbab-Zadeh A, Prasad A, Okazaki K, Levine BD. Persistent sympathetic activation during chronic antihypertensive therapy: a potential mechanism for long term morbidity. Hypertension. 2005;45:513-521. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 60] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 26. | Liang WW. Seasonal changes in preprandial glucose, A1C, and blood pressure in diabetic patients. Diabetes Care. 2007;30:2501-2502. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 54] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 27. | Niimi Y, Matsukawa T, Sugiyama Y, Shamsuzzaman AS, Mano T. Comparison [correction of Compariso] of sympathetic nerve response to head-up tilt in summer [correction of sumer] and winter. J Gravit Physiol. 1999;6:P43-P44. [PubMed] [Cited in This Article: ] |
| 28. | Rosenthal T. Seasonal variations in blood pressure. Am J Geriatr Cardiol. 2004;13:267-272. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 29. | Bi SH, Cheng LT, Zheng DX, Wang T. Seasonal changes in blood pressure in chronic kidney disease patients. Clin Nephrol. 2010;73:216-220. [PubMed] [Cited in This Article: ] |
| 30. | Youn JC, Rim SJ, Park S, Ko YG, Kang SM, Choi D, Ha JW, Jang Y, Chung N. Arterial stiffness is related to augmented seasonal variation of blood pressure in hypertensive patients. Blood Press. 2007;16:375-380. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 31. | El-Hajj H, Oriowo MA. Effect of chronic exposure to cold on isoprenaline-induced cAMP accumulation and relaxation in the rat aorta. Life Sci. 2006;78:592-597. [PubMed] [Cited in This Article: ] |
| 32. | Liu J, Cao TS, Duan YY, Yang YL, Yuan LJ. Effects of cold pressor-induced sympathetic stimulation on the mechanical properties of common carotid and femoral arteries in healthy males. Heart Vessels. 2011;26:214-221. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 33. | Radke KJ, Izzo JL. Seasonal variation in haemodynamics and blood pressure-regulating hormones. J Hum Hypertens. 2010;24:410-416. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 34. | Hirvonen J, Lindeman S, Matti J, Huttunen P. Plasma catecholamines, serotonin and their metabolites and beta-endorphin of winter swimmers during one winter. Possible correlations to psychological traits. Int J Circumpolar Health. 2002;61:363-372. [PubMed] [Cited in This Article: ] |
| 35. | Perini R, Tironi A, Cautero M, Di Nino A, Tam E, Capelli C. Seasonal training and heart rate and blood pressure variabilities in young swimmers. Eur J Appl Physiol. 2006;97:395-403. [PubMed] [Cited in This Article: ] |
| 36. | Yamazaki F. [Heat stress and human baroreflex function]. J UOEH. 2010;32:329-340. [PubMed] [Cited in This Article: ] |
| 37. | Sarna S, Romo M, Siltanen P. Myocardial infarction and weather. Ann Clin Res. 1977;9:222-232. [PubMed] [Cited in This Article: ] |
| 38. | Goldstein MR, Mascitelli L, Pezzetta F. Regarding the inverse relationship between blood pressure and outdoor temperature: it is the sun. Arch Intern Med. 2009;169:1167. [PubMed] [Cited in This Article: ] |
| 39. | Keller MC, Fredrickson BL, Ybarra O, Côté S, Johnson K, Mikels J, Conway A, Wager T. A warm heart and a clear head. The contingent effects of weather on mood and cognition. Psychol Sci. 2005;16:724-731. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 231] [Cited by in F6Publishing: 116] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 40. | Delfino RJ, Tjoa T, Gillen DL, Staimer N, Polidori A, Arhami M, Jamner L, Sioutas C, Longhurst J. Traffic-related air pollution and blood pressure in elderly subjects with coronary artery disease. Epidemiology. 2010;21:396-404. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 141] [Cited by in F6Publishing: 146] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 41. | Rintamäki R, Grimaldi S, Englund A, Haukka J, Partonen T, Reunanen A, Aromaa A, Lönnqvist J. Seasonal changes in mood and behavior are linked to metabolic syndrome. PLoS One. 2008;3:e1482. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 51] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 42. | Sinha P, Kumar TD, Singh NP, Saha R. Seasonal variation of blood pressure in normotensive females aged 18 to 40 years in an urban slum of Delhi, India. Asia Pac J Public Health. 2010;22:134-145. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 43. | Ulmer H, Kelleher C, Diem G, Concin H, Ruttmann E. Estimation of seasonal variations in risk factor profiles and mortality from coronary heart disease. Wien Klin Wochenschr. 2004;116:662-668. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 32] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 44. | Halonen JI, Zanobetti A, Sparrow D, Vokonas PS, Schwartz J. Associations between outdoor temperature and markers of inflammation: a cohort study. Environ Health. 2010;9:42. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 95] [Cited by in F6Publishing: 55] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 45. | Weiss A, Beloosesky Y, Grinblat J, Grossman E. Seasonal changes in orthostatic hypotension among elderly admitted patients. Aging Clin Exp Res. 2006;18:20-24. [PubMed] [Cited in This Article: ] |
| 46. | Bailey SR, Katz LM, Berhane Y, Samuels T, De Brauvere N, Marr CM, Elliott J. Seasonal changes in plasma concentrations of cecum-derived amines in clinically normal ponies and ponies predisposed to laminitis. Am J Vet Res. 2003;64:1132-1138. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 47. | Modesti PA, Morabito M, Bertolozzi I, Massetti L, Panci G, Lumachi C, Giglio A, Bilo G, Caldara G, Lonati L. Weather-related changes in 24-hour blood pressure profile: effects of age and implications for hypertension management. Hypertension. 2006;47:155-161. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 162] [Cited by in F6Publishing: 159] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 48. | Lanska DJ, Hoffmann RG. Seasonal variation in stroke mortality rates. Neurology. 1999;52:984-990. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 71] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 49. | Cui ZH, Ikeda K, Kawakami K, Gonda T, Masuda J, Nabika T. Exaggerated response to cold stress in a congenic strain for the quantitative trait locus for blood pressure. J Hypertens. 2004;22:2103-2109. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 50. | Tienviboon C, Punyagupta S, Pongtarakulpanit A, Prichanond S. Reversible cerebral vasoconstriction syndrome with increased intracranial pressure, probably related to altitude changes and windy winter travelling. J Med Assoc Thai. 2011;94:622-628. [PubMed] [Cited in This Article: ] |
| 51. | Pedelty L, Gorelick PB. Management of hypertension and cerebrovascular disease in the elderly. Am J Med. 2008;121:S23-S31. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 52. | Goodwin J, Pearce VR, Taylor RS, Read KL, Powers SJ. Seasonal cold and circadian changes in blood pressure and physical activity in young and elderly people. Age Ageing. 2001;30:311-317. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 44] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 53. | Healy JD. Excess winter mortality in Europe: a cross country analysis identifying key risk factors. J Epidemiol Community Health. 2003;57:784-789. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 390] [Cited by in F6Publishing: 262] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 54. | Seto TB, Mittleman MA, Davis RB, Taira DA, Kawachi I. Seasonal variation in coronary artery disease mortality in Hawaii: observational study. BMJ. 1998;316:1946-1947. [PubMed] [Cited in This Article: ] |
| 55. | Wolf K, Schneider A, Breitner S, von Klot S, Meisinger C, Cyrys J, Hymer H, Wichmann HE, Peters A. Air temperature and the occurrence of myocardial infarction in Augsburg, Germany. Circulation. 2009;120:735-742. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 151] [Cited by in F6Publishing: 156] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 56. | Díaz A, Gerschcovich ER, Díaz AA, Antía F, Gonorazky S. Seasonal Variation and Trends in Stroke Hospitalizations and Mortality in a South American Community Hospital. J Stroke Cerebrovasc Dis. 2012;Epub ahead of print. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 57. | Myint PK, Vowler SL, Woodhouse PR, Redmayne O, Fulcher RA. Winter excess in hospital admissions, in-patient mortality and length of acute hospital stay in stroke: a hospital database study over six seasonal years in Norfolk, UK. Neuroepidemiology. 2007;28:79-85. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 44] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 58. | Medina-Ramón M, Schwartz J. Temperature, temperature extremes, and mortality: a study of acclimatisation and effect modification in 50 US cities. Occup Environ Med. 2007;64:827-833. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 367] [Cited by in F6Publishing: 299] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 59. | Basu R, Dominici F, Samet JM. Temperature and mortality among the elderly in the United States: a comparison of epidemiologic methods. Epidemiology. 2005;16:58-66. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 123] [Cited by in F6Publishing: 128] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 60. | Braga AL, Zanobetti A, Schwartz J. The time course of weather-related deaths. Epidemiology. 2001;12:662-667. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 289] [Cited by in F6Publishing: 251] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 61. | Cold exposure and winter mortality from ischaemic heart disease, cerebrovascular disease, respiratory disease, and all causes in warm and cold regions of Europe. The Eurowinter Group. Lancet. 1997;349:1341-1346. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 625] [Cited by in F6Publishing: 518] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 62. | Morabito M, Modesti PA, Cecchi L, Crisci A, Orlandini S, Maracchi G, Gensini GF. Relationships between weather and myocardial infarction: a biometeorological approach. Int J Cardiol. 2005;105:288-293. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 81] [Cited by in F6Publishing: 82] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 63. | Liang WM, Liu WP, Chou SY, Kuo HW. Ambient temperature and emergency room admissions for acute coronary syndrome in Taiwan. Int J Biometeorol. 2008;52:223-229. [PubMed] [Cited in This Article: ] |
| 64. | Ye F, Piver WT, Ando M, Portier CJ. Effects of temperature and air pollutants on cardiovascular and respiratory diseases for males and females older than 65 years of age in Tokyo, July and August 1980-1995. Environ Health Perspect. 2001;109:355-359. [PubMed] [Cited in This Article: ] |
| 65. | Gerber Y, Jacobsen SJ, Killian JM, Weston SA, Roger VL. Seasonality and daily weather conditions in relation to myocardial infarction and sudden cardiac death in Olmsted County, Minnesota, 1979 to 2002. J Am Coll Cardiol. 2006;48:287-292. [PubMed] [Cited in This Article: ] |
| 66. | Barnett AG, Dobson AJ, McElduff P, Salomaa V, Kuulasmaa K, Sans S. Cold periods and coronary events: an analysis of populations worldwide. J Epidemiol Community Health. 2005;59:551-557. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 175] [Cited by in F6Publishing: 161] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 67. | Chang CL, Shipley M, Marmot M, Poulter N. Lower ambient temperature was associated with an increased risk of hospitalization for stroke and acute myocardial infarction in young women. J Clin Epidemiol. 2004;57:749-757. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 79] [Cited by in F6Publishing: 82] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 68. | Spencer FA, Goldberg RJ, Becker RC, Gore JM. Seasonal distribution of acute myocardial infarction in the second National Registry of Myocardial Infarction. J Am Coll Cardiol. 1998;31:1226-1233. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 331] [Cited by in F6Publishing: 330] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 69. | Pell JP, Cobbe SM. Seasonal variations in coronary heart disease. QJM. 1999;92:689-696. [PubMed] [Cited in This Article: ] |
| 70. | Green MS, Gil Harari G, Kristal-Boneh E. Excess winter mortality from ischaemic heart disease and stroke during colder and warmer years in Israel. An evaluation and review of the role of environmental temperature. Eur J Public Health. 1994;4:3-11. [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 21] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 71. | Douglas S, Rawles J. Latitude-related changes in the amplitude of annual mortality rhythm. The biological equator in man. Chronobiol Int. 1999;16:199-212. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 72. | Enquselassie F, Dobson AJ, Alexander HM, Steele PL. Seasons, temperature and coronary disease. Int J Epidemiol. 1993;22:632-636. [Cited in This Article: ] |