Abstract
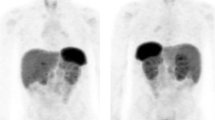
Combining anatomical and functional imaging can improve sensitivity and accuracy of tumor diagnosis and surveillance of pediatric malignancies. MRI is the state-of-the-art modality for demonstrating the anatomical location of brain tumors with contrast enhancement adding additional information regarding whether the tumor is neuronal or glial. Addition of SPECT imaging using a peptide that targets the somatostatin receptor (Octreoscan) can now differentiate medulloblastoma from a cerebellar pilocytic astrocytoma. Combined MRI and Octreoscan is now the most sensitive and accurate imaging modality for differentiating recurrent medulloblastoma from scar tissue. CT is the most common imaging modality for demonstrating the anatomical location of tumors in the chest and abdomen. Addition of SPECT imaging with either MIBG or Octreoscan has been shown to add important diagnostic information on the nature of tumors in chest and abdomen and is often more sensitive than CT for identification of metastatic lesions in bone or liver. Combined anatomical and functional imaging is particularly helpful in neuroblastoma and in neuroendocrine tumors such as gastrinoma and carcinoid. Functional imaging with MIBG and Octreoscan is predictive of response to molecularly targeted therapy with 131I-MIBG and 90Y-DOTA-tyr3-Octreotide. Dosimetry using combined anatomical and functional imaging is being developed for patient-specific dosing of targeted radiotherapy and as an extremely sensitive monitor of response to therapy. Both MIBG and Octreotide are now being adapted to PET imaging which will greatly improve the utility of PET in medulloblastoma as well as increase the sensitivity for detection of metastatic lesions in neuroblastoma and neuroendocrine tumors.











Similar content being viewed by others
References
Heideman, R. L., Packer, R. J., Albright, L. A., Freeman, C. R., & Rorke, L. B. (1997). In P. A. Pizzo, & D. G. Poplack (Eds.), Principles and practice of pediatric oncology pp. 633–697. Philadelphia: Lippincott-Raven.
Hirakawa, K., Suzuki, K., Ueda, S., & Handa, J. (1986). Fetal origin of the medulloblastoma: Evidence from growth analysis of two cases. Acta Neuropathologica (Berl), 70(3–4), 227–234.
Yachnis, A. T., Rorke, L. B., & Trojanowski, J. Q. (1994). Cerebellar dysplasias in humans: Development and possible relationship to glial and primitive neuroectodermal tumors of the cerebellar vermis. Journal of Neuropathology and Experimental Neurology, 53(1), 61–71.
Scherini, E., & Bernocchi, G. (1994). CisDDP treatment and development of the rat cerebellum. Progress in Neurobiology, 42(2), 161–196.
Zhang, L., & Goldman, J. E. (1996). Generation of cerebellar interneurons from dividing progenitors in white matter. Neuron, 16(1), 47–54.
Rubinstein, L. J. (1985). Embryonal central neuroepithelial tumors and their differentiating potential. A cytogenetic view of a complex neuro-oncological problem. Journal of Neurosurgery, 62(6), 795–805.
Bailey, P., & Cushing, H. (1925). Medulloblastoma cerebelli: A common type of midcerebellar glioma of childhood. Archives of Neurology and Psychiatry, 14, 192–224.
Trojanowski, J. Q., Tohyama, T., & Lee, V. M. (1992). Medulloblastomas and related primitive neuroectodermal brain tumors of childhood recapitulate molecular milestones in the maturation of neuroblasts. Molecular and Chemical Neuropathology, 17(2), 121–135.
Packer, R. J. (1999). Childhood medulloblastoma: Progress and future challenges. Brain & Development, 21(2), 75–81.
Gurney, J. G., Kadan-Lottick, N. S., Packer, R. J., Neglia, J. P., Sklar, C. A., Punyko, J. A., et al. (2003). Endocrine and cardiovascular late effects among adult survivors of childhood brain tumors: Childhood Cancer Survivor Study. Cancer, 97(3), 663–673.
Fangusaro, J., Finlay, J., Sposto, R., Ji, L., Saly, M., Zacharoulis, S., et al. (2007). Intensive chemotherapy followed by consolidative myeloablative chemotherapy with autologous hematopoietic cell rescue (AuHCR) in young children with newly diagnosed supratentorial primitive neuroectodermal tumors (sPNETs): Report of the Head Start I and II experience. Pediatr Blood Cancer.
Bull, K. S., Spoudeas, H. A., Yadegarfar, G., & Kennedy, C. R. (2007). Reduction of health status 7 years after addition of chemotherapy to craniospinal irradiation for medulloblastoma: A follow-up study in PNET 3 trial survivors on behalf of the CCLG (formerly UKCCSG). Journal of Clinical Oncology, 25(27), 4239–4245.
Polkinghorn, W. R., & Tarbell, N. J. (2007). Medulloblastoma: Tumorigenesis, current clinical paradigm, and efforts to improve risk stratification. Nat Clin Pract Oncol, 4(5), 295–304.
Dennis, M., Spiegler, B. J., Hetherington, C. R., & Greenberg, M. L. (1996). Neuropsychological sequelae of the treatment of children with medulloblastoma. Journal of Neuro-oncology, 29(1), 91–101.
Hoppe-Hirsch, E., Brunet, L., Laroussinie, F., Cinalli, G., Pierre-Kahn, A., Renier, D., et al. (1995). Intellectual outcome in children with malignant tumors of the posterior fossa: Influence of the field of irradiation and quality of surgery. Child’s Nervous System, 11(6), 340–345.
David, K. M., Casey, A. T., Hayward, R. D., Harkness, W. F., Phipps, K., & Wade, A. M. (1997). Medulloblastoma: Is the 5-year survival rate improving? A review of 80 cases from a single institution. Journal of Neurosurgery, 86(1), 13–21.
Khanna, G., O’Dorisio, M. S., Menda, Y., Glasier, C., Deyoung, B., Smith, B. J., et al. (2007). Somatostatin receptor scintigraphy in surveillance of pediatric brain malignancies. Pediatric Blood and Cancer, 50, 561–566.
Biegel, J. A. (1997). Genetics of pediatric central nervous system tumors. Journal of Pediatric Hematology Oncology, 19(6), 492–501.
Wilgenbus, K. K., Seranski, P., Brown, A., Leuchs, B., Mincheva, A., Lichter, P., et al. (1997). Molecular characterization of a genetically unstable region containing the SMS critical area and a breakpoint cluster for human PNETs. Genomics, 42(1), 1–10.
Bigner, S. H., & Schrock, E. (1997). Molecular cytogenetics of brain tumors. Journal of Neuropathology and Experimental Neurology, 56(11), 1173–1181.
MacGregor, D. N., & Ziff, E. B. (1990). Elevated c-myc expression in childhood medulloblastomas. Pediatric Research, 28(1), 63–68 Ref Type: Abstract.
Fruhwald, M. C., O’Dorisio, M. S., Rush, L. J., Reiter, J. L., Smiraglia, D. J., Wenger, G., et al. (2000). Gene amplification in PNETs/medulloblastomas: Mapping of a novel amplified gene within the MYCN amplicon. Journal of Medical Genetics, 37(7), 501–509.
Goodrich, L. V., Milenkovic, L., Higgins, K. M., & Scott, M. P. (1997). Altered neural cell fates and medulloblastoma in mouse patched mutants. Science, 277(5329), 1109–1113.
Pietsch, T., Waha, A., Koch, A., Kraus, J., Albrecht, S., Tonn, J., et al. (1997). Medulloblastomas of the desmoplastic variant carry mutations of the human homologue of Drosophila patched. Cancer Research, 57(11), 2085–2088.
Zakrzewska, M., Rieske, P., biec-Rychter, M., Zakrzewski, K., Polis, L., Fiks, T., et al. (2004). Molecular abnormalities in pediatric embryonal brain tumors-analysis of loss of heterozygosity on chromosomes 1, 5, 9, 10, 11, 16, 17 and 22. Clinical Neuropathology, 23(5), 209–217.
Wolter, M., Reifenberger, J., Sommer, C., Ruzicka, T., & Reifenberger, G. (1997). Mutations in the human homologue of the Drosophila segment polarity gene patched (PTCH) in sporadic basal cell carcinomas of the skin and primitive neuroectodermal tumors of the central nervous system. Cancer Research, 57(13), 2581–2585.
Uziel, T., Zindy, F., Xie, S., Lee, Y., Forget, A., Magdaleno, S., et al. (2005). The tumor suppressors Ink4c and p53 collaborate independently with Patched to suppress medulloblastoma formation. Genes & Development, 19(22), 2656–2667.
Zindy, F., Uziel, T., Ayrault, O., Calabrese, C., Valentine, M., Rehg, J. E., et al. (2007). Genetic alterations in mouse medulloblastomas and generation of tumors de novo from primary cerebellar granule neuron precursors. Cancer Research, 67(6), 2676–2684.
Muhlisch, J., Bajanowski, T., Rickert, C. H., Roggendorf, W., Wurthwein, G., Jurgens, H., et al. (2007). Frequent but borderline methylation of p16 (INK4a) and TIMP3 in medulloblastoma and sPNET revealed by quantitative analyses. Journal of Neuro-oncology, 83(1), 17–29.
Sardi, I., Cavalieri, D., & Massimino, M. (2007). Emerging treatments and gene expression profiling in high-risk medulloblastoma. Paediatric Drugs, 9(2), 81–96.
Brodeur, G. M., & Maris, J. M. (2001). In P. A. Pizzo, & D. G. Poplack (Eds.), Principles and practice of pediatric oncology pp. 895–937. Philadelphia: Lippincott Williams & Wilkins.
Thiele, C. J. (1991). Biology of pediatric peripheral neuroectodermal tumors. Cancer Metastasis Reviews, 10(4), 311–319.
Dehner, L. P. (1993). Primitive neuroectodermal tumor and Ewing’s sarcoma. American Journal of Surgical Pathology, 17(1), 1–13.
Kitlinska, J., Abe, K., Kuo, L., Pons, J., Yu, M., Li, L., et al. (2005). Differential effects of neuropeptide Y on the growth and vascularization of neural crest-derived tumors. Cancer Research, 65(5), 1719–1728.
Matthay, K. K., Villablanca, J. G., Seeger, R. C., Stram, D. O., Harris, R. E., Ramsay, N. K., et al. (1999). Treatment of high-risk neuroblastoma with intensive chemotherapy, radiotherapy, autologous bone marrow transplantation, and 13-cis-retinoic acid. Children’s Cancer Group. New England Journal of Medicine, 341(16), 1165–1173.
Altungoz, O., Aygun, N., Tumer, S., Ozer, E., Olgun, N., & Sakizli, M. (2007). Correlation of modified Shimada classification with MYCN and 1p36 status detected by fluorescence in situ hybridization in neuroblastoma. Cancer Genetics and Cytogenetics, 172(2), 113–119.
Gurcan, M. N., Pan, T., Shimada, H., & Saltz, J. (2006). Image analysis for neuroblastoma classification: Segmentation of cell nuclei. Conference Proceedings of IEEE Engineering in Medicine and Biology Society, 1, 4844–4847.
Brodeur, G. M., Seeger, R. C., Schwab, M., Varmus, H. E., & Bishop, J. M. (1984). Amplification of N-myc in untreated human neuroblastomas correlates with advanced disease stage. Science, 224(4653), 1121–1124.
Sano, H., Bonadio, J., Gerbing, R. B., London, W. B., Matthay, K. K., Lukens, J. N., et al. (2006). International neuroblastoma pathology classification adds independent prognostic information beyond the prognostic contribution of age. European Journal of Cancer, 42(8), 1113–1119.
Modlin, I. M., Kidd, M., Latich, I., Zikusoka, M. N., Eick, G. N., Mane, S. M., et al. (2006). Genetic differentiation of appendiceal tumor malignancy: A guide for the perplexed. Annals of Surgery, 244(1), 52–60.
Stinner, B., & Rothmund, M. (2005). Neuroendocrine tumours (carcinoids) of the appendix. Best Pract Res Clin Gastroenterol, 19(5), 729–738.
Khanna, G., O’Dorisio, M. S., Menda, Y., Kirby, P., Kao, S., & Sato, Y. (2007). Gastroenteropancreatic Neuroendocrine Tumors in Children and Young Adults. Pediatric Radiology, 38, 251–259.
SEER Cancer Statistics Review, 1973–2004. 1-11-2006. Ref Type: Report
Vinik, A. I., Thompson, N., Eckhauser, F., & Moattari, A. R. (1989). Clinical features of carcinoid syndrome and the use of somatostatin analogue in its management. Acta Oncologica, 28(3), 389–402.
Lamberts, S. W., Pieters, G. F., Metselaar, H. J., Ong, G. L., Tan, H. S., & Reubi, J. C. (1988). Development of resistance to a long-acting somatostatin analogue during treatment of two patients with metastatic endocrine pancreatic tumours. Acta Endocrinologica (Copenh), 119(4), 561–566.
McDermott, E. W., Guduric, B., & Brennan, M. F. (1994). Prognostic variables in patients with gastrointestinal carcinoid tumours. British Journal of Surgery, 81(7), 1007–1009.
Broaddus, R. R., Herzog, C. E., & Hicks, M. J. (2003). Neuroendocrine tumors (carcinoid and neuroendocrine carcinoma) presenting at extra-appendiceal sites in childhood and adolescence. Archives of Pathology and Laboratory Medicine, 127(9), 1200–1203.
Pashankar, F. D., O’Dorisio, M. S., & Menda, Y. (2005). MIBG and somatostatin receptor analogs in children: Current concepts on diagnostic and therapeutic use. Journal of Nuclear Medicine, 46(Suppl 1), 55S–61S.
Kloppel, G. PAHP. (2004). The gastroenteropancreatic neuroendocrine cell system and its tumors: The WHO classification. Annals of the New York Academy of Sciences, 1014, 13–27 Ref Type: Generic.
Rindi, G., Kloppel, G., Alhman, H., Caplin, M., Couvelard, A., de Herder, W. W., et al. (2006). TNM staging of foregut (neuro)endocrine tumors: A consensus proposal including a grading system. Virchows Archives, 449(4), 395–401.
Modlin, I. M., Lye, K. D., & Kidd, M. (2003). A 5-decade analysis of 13,715 carcinoid tumors. Cancer, 97(4), 934–959.
Bonato, M., Cerati, M., Pagani, A., Papotti, M., Bosi, F., Bussolati, G., et al. (1992). Differential diagnostic patterns of lung neuroendocrine tumours. A clinico-pathological and immunohistochemical study of 122 cases. Virchows Archiv. A, Pathological Anatomy and Histopathology, 420(3), 201–211.
Modlin, I. M., Kidd, M., Pfragner, R., Eick, G. N., & Champaneria, M. C. (2006). The functional characterization of normal and neoplastic human enterochromaffin cells. Journal of Clinical Endocrinology and Metabolism, 91(6), 2340–2348.
Kulke, M. H., & Mayer, R. J. (1999). Carcinoid tumors. New England Journal of Medicine, 340(11), 858–868.
Rindi, G., Capella, C., Bordi, C., & Solcia, E. (2002). Guidelines and minimal diagnostic criteria for the histological diagnosis of endocrine tumors of the gastroenteropancreatic type. Pathologica, 94(3), 142–147.
Fiocca, R., Rindi, G., Capella, C., Grimelius, L., Polak, J. M., Schwartz, T. W., et al. (1987). Glucagon, glicentin, proglucagon, PYY, PP and proPP-icosapeptide immunoreactivities of rectal carcinoid tumors and related non-tumor cells. Regulatory Peptide, 17(1), 9–29.
Shankar, L. K., Hoffman, J. M., Bacharach, S., Graham, M. M., Karp, J., Lammertsma, A. A., et al. (2006). Consensus recommendations for the use of 18F-FDG PET as an indicator of therapeutic response in patients in National Cancer Institute Trials. Journal of Nuclear Medicine, 47(6), 1059–1066.
Ott, R. J., Tait, D., Flower, M. A., Babich, J. W., & Lambrecht, R. M. (1992). Treatment planning for 131I-mIBG radiotherapy of neural crest tumours using 124I-mIBG positron emission tomography. British Journal of Radiology, 65(777), 787–791.
Maecke, H. R., Hofmann, M., & Haberkorn, U. (2005). (68)Ga-labeled peptides in tumor imaging. Journal of Nuclear Medicine, 46(Suppl 1), 172S–178S.
Nataf, V., Balard, M., de B, V., Kerrou, K., Gutman, F., Grahek, D., et al. (2006). Safety of 18F-DOPA Injection for PET of Carcinoid Tumor. Journal of Nuclear Medicine, 47(10), 1732.
Juweid, M. E., Wiseman, G. A., Vose, J. M., Ritchie, J. M., Menda, Y., Wooldridge, J. E., et al. (2005). Response assessment of aggressive non-Hodgkin’s lymphoma by integrated International Workshop Criteria and fluorine-18-fluorodeoxyglucose positron emission tomography. Journal of Clinical Oncology, 23(21), 4652–4661.
Howard, J. P., Maris, J. M., Kersun, L. S., Huberty, J. P., Cheng, S. C., Hawkins, R. A., et al. (2005). Tumor response and toxicity with multiple infusions of high dose 131I-MIBG for refractory neuroblastoma. Pediatric Blood and Cancer, 44(3), 232–239.
Rose, B., Matthay, K. K., Price, D., Huberty, J., Klencke, B., Norton, J. A., et al. (2003). High-dose 131I-metaiodobenzylguanidine therapy for 12 patients with malignant pheochromocytoma. Cancer, 98(2), 239–248.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
O’Dorisio, M.S., Khanna, G. & Bushnell, D. Combining anatomic and molecularly targeted imaging in the diagnosis and surveillance of embryonal tumors of the nervous and endocrine systems in children. Cancer Metastasis Rev 27, 665–677 (2008). https://doi.org/10.1007/s10555-008-9153-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-008-9153-8