Abstract
Purpose
The aim of this study was to identify baseline features that predict outcome in 223Ra therapy.
Methods
We retrospectively reviewed 110 patients with metastatic castration-resistant prostate cancer treated with 223Ra. End points were overall survival (OS), progression-free survival (PFS), bone event-free survival (BeFS), and bone marrow failure (BMF). The following parameters were evaluated prior to the first 223Ra cycle: serum levels of hemoglobin (Hb), prostate-specific antigen (PSA), alkaline phosphatase (ALP), Eastern Cooperative Oncology Group (ECOG) status, pain score, use of chemotherapy, and external beam radiation therapy (EBRT). During/after 223Ra we evaluated: the total number of radium cycles (RaTot), the PSA doubling time (PSADT), and the use of chemotherapy, EBRT, abiraterone, and enzalutamide.
Results
A significant reduction of ALP (p < 0.001) and pain score (p = 0.041) occurred throughout the 223 Ra cycles. The risk of progression was associated with declining ECOG status [hazard ratio (HR) = 3.79; p < 0.001] and decrease in PSADT (HR = 8.22; p < 0.001). RaTot, ALP, initial ECOG status, initial pain score, and use of abiraterone were associated with OS (p ≤ 0.008), PFS (p ≤ 0.003), and BeFS (p ≤ 0.020). RaTot, ALP, initial ECOG status, and initial pain score were significantly associated with BMF (p ≤ 0.001) as well as Hb (p < 0.001) and EBRT (p = 0.009). On multivariable analysis, only RaTot and abiraterone remained significantly associated with OS (p < 0.001; p = 0.033, respectively), PFS (p < 0.001; p = 0.041, respectively), and BeFS (p < 0.001; p = 0.019, respectively). Additionally, RaTot (p = 0.027) and EBRT (p = 0.013) remained significantly associated with BMF.
Conclusion
Concomitant use of abiraterone and 223Ra seems to have a beneficial effect, while the EBRT may increase the risk of BMF.
Similar content being viewed by others
Introduction
Radium dichloride therapy (223Ra) is gaining widespread use in patients with symptomatic bone metastases from castration-resistant prostate cancer (mCRPC) due to its demonstrated survival benefits [1–3]. However, outside of controlled regulatory trials, the algorithm and therapeutic approach of this novel radiopharmaceutical are not well established.
Bone-related parameters are typically used to predict overall survival (OS) in mCRPC patients [4]. Worst survival is observed in patients with hemoglobin (Hb) levels below 10 g/dl, prostate-specific antigen (PSA) levels above 10 ng/ml, alkaline phosphatase (ALP) levels above 146 U/l, pain scores above 3 (according to the WHO criteria), the presence of skeletal-related events, patients with older age, and patients with visceral metastases. However, when managing mCRPC patients in the compassionate scenario, many (if not all) of the bone-related parameters frequently used to determine outcome denote dismal survival in all patients, and thus the discrimination of which patients benefit from therapy in terms of OS, progression-free survival (PFS), marrow depletion, and skeletal-related events is more difficult. As a result, there is a need to identify factors that will predict outcome, especially for new therapies, like 223Ra.
Given that the therapeutic approach of 223Ra is not well established in clinical practice, to obtain the full benefit of this novel therapy in mCRPC patients, there is a need to establish the optimal time to perform 223Ra as these patients with rapidly progressing tumors may not have sufficient time for marrow recovery prior to their next 223Ra treatment. Likewise, it is important to determine which factors, such as combined therapies and disease status, may influence 223Ra treatment.
Although there have been previous reports on 223Ra with a limited number of patients and with a short follow-up [5], to our knowledge there have not been reports from a single institution with a large number of patients treated with 223Ra outside a regulatory trial. Consequently, it is not clear where 223Ra should be placed in the treatment algorithm for mCRPC patients, especially in the clinical setting of a compassionate use program. The purpose of this study was to determine the factors that may predict outcome in patients undergoing 223Ra therapy.
Materials and methods
Study design
This retrospective study was approved by our Institutional Review Board (PA14-0848). The waivers of informed consent and authorization were granted for the retrospective analysis. We reviewed records of consecutive patients with histologically confirmed mCRPC treated with 223Ra between July 2013 and March 2015.
Clinical and laboratory evaluation prior to 223Ra
Clinical evaluation prior to 223Ra consisted of determining the patient’s Eastern Cooperative Oncology Group (ECOG) performance status and pain scores (according to WHO criteria) (Table 1).
Laboratory tests prior to 223Ra involved assessing the patient’s hematologic status and the dynamics of the disease. These consisted of serum concentrations of Hb, platelets (PLT), absolute neutrophil counts (ANC), ALP, and PSA. Laboratory parameter cutoff values established to determine the ability to predict survival [4, 6] were as follows: Hb <10 g/dl vs ≥10 g/dl, ALP ≥146 UI/l vs <146 UI/l, and PSA >10 ng/ml vs ≤ 10 ng/ml. The clinical and laboratory parameters evaluated prior to the first 223Ra cycle were: Hb, PSA, ALP, ECOG status, pain scores, and the use of chemotherapy and external beam radiation therapy (EBRT). During and/or after the 223Ra cycles the clinical and laboratory parameters assessed were: total number of radium cycles (RaTot) and use of chemotherapy, EBRT, abiraterone, and enzalutamide. In addition, PSA doubling time (PSADT) was computed between two 233Ra cycles and the cutoff used to predict survival was <3 months vs ≥3 months.
Imaging evaluation prior to 223Ra
Imaging studies were performed on all patients prior to 223Ra. These studies consisted of one or more of the following in order to determine eligibility for 223Ra therapy and/or to restage the patients: whole-body skeletal 18F-fluoride positron emission tomography (PET)/CT scan (69.1 %), whole-body metabolic 18F-fluorodeoxyglucose (FDG) PET/CT scan (23.6 %), and whole-body conventional bone scintigraphy (7.3 %). In addition, some patients had CT scans and MRI scans per standard clinical practice. In some cases, biopsy was performed in order to determine the etiology of equivocal lesions, again based on clinical decisions.
Skeletal tumor burden was classified as low, intermediate, and high burden. In patients imaged with 18F-fluoride PET/CT scans and whole-body conventional bone scintigraphy, skeletal tumor burden was classified as low when the number of bone metastases was less than 20, intermediate when the number of bone metastases was between 20 and 50, and high when the number of bone metastases was above 50 or in the presence of diffuse disease (superscan). On whole-body metabolic 18F-FDG PET/CT scans the metabolic tumor burden was classified as low when the number of metabolically active bone metastases was less than 6, intermediate when the number of bone metastases was between 6 and 20, and high when the number of bone metastases was above 20.
Determination of outcome measures
The primary end point was OS, which was established from initial 223Ra dose until date of death from any cause or last follow-up. Patients alive at the last follow-up date were censored. Secondary end points were PFS, bone event-free survival (BeFS), time to progression (TTP), and bone marrow failure (BMF). Patients who were alive and did not experience an event (progression, bone event, or BMF) were censored. PFS was established from initial 223Ra cycle until date of objective tumor progression, death of any cause, or last follow-up. Objective tumor progression was defined as a lesion progressing in the bone or soft tissue (nodal or visceral lesions) leading to a change in current therapy or initiation of another therapy (chemotherapy, radiation therapy, or secondary hormone therapy). TTP was assessed from the date of initial 223Ra cycle to date of objective tumor progression. BeFS was defined from initial 223Ra cycle until the date of an objective skeletal-related event, characterized as a surgical intervention, spinal cord compression, pathologic fracture, bone pain or rapid lesion progression requiring immediate intervention, death of any cause, or last follow-up. BMF was assessed from the date of last 223Ra cycle to date of BMF. BMF was defined as: (1) the development of hematologic toxicity (WHO grades 3 or 4) (Table 1) associated with no recovery after 6 weeks or (2) death due to BMF after the last 223Ra cycle.
223Ra treatment
223Ra treatment was performed in 110 mCRPC patients. All patients had bone metastases; additionally, 36 % of these patients had visceral and/or nodal metastases. All patients completed between one and sicx cycles of 223Ra.
Eligibility criteria for treatment with 223Ra consisted of being older than 18 years and signing the informed consent. In addition, it was necessary to have ANC > 1.5 K/μl and PLT > 100 K/uμl Hb levels below 10 g/dl were not an exclusion criterion and patients with lower Hb levels were transfused prior to 223Ra. Intravenous infusions of 50 kBq/kg (1.4 μCi/kg) of 223RaCl2 doses were injected every 4 weeks. Prior to next the 223Ra cycle, ANC had to be above 1.0 K/μl and PLT > 50 K/μl. After each 223Ra cycle, the patients were counseled regarding expected side effects and precautions of the radiopharmaceutical.
Statistical methods
Patient and clinical characteristics were summarized using descriptive statistics. Associations between 223Ra cycles over time and pain scores as well as ALP levels were evaluated using repeated measures analysis of variance with an unstructured covariance matrix.
Survival times were estimated using the Kaplan-Meier method. Associations between OS, PFS, TTP, BeFS and BMF and clinical measures of interest were determined using univariable and multivariable Cox proportional hazards regression models. Treatments received (chemotherapy, EBRT, and secondary hormonal therapy) and measures obtained (ECOG status and PSADT over 223Ra treatment) after the start time of each survival outcome were included in the Cox models as time-dependent covariates. The PSADT was computed in two ways: (1) for each consecutive PSA value and (2) for the first and last PSA values. Of note, the start date for all survival outcomes in the assessment for PSADT from initial to final value was the last 223Ra cycle date. The following formula [6] was used to compute PSADT:
All statistical analyses were performed using SAS 9.3 for Windows (© 2011 by SAS Institute Inc., Cary, NC, USA). All statistical tests used a significance level of 5 %. No adjustments for multiple testing were made.
Results
The median age of the mCRPC patients prior to their first 223Ra cycle was 69.0 years (42.4–88.1 years); the median follow-up time was 8.3 months (0.4–18.4 months).
223Ra cycles and time-to-event outcome measures
A total of 532 223Ra doses were delivered to 110 patients. The details on patient characteristics are described in Table 2. 223Ra cycles ranged from 1 to 6 (mean = 5). These cycles were completed in 58 (53 %) patients, while 4 patients (4 %) were still undergoing 223Ra treatment at the time of analysis. The planned course of six infusions of 223Ra was interrupted in 48 patients (44 %) due to progression and one or more of the following: hematologic toxicity (n = 22), declining ECOG status by two points (n = 20), or a skeletal-related event (n = 11).
The median [95 % confidence interval (CI)] OS time was 11.7 (8.6–15.7) months, PFS was 4.3 (3.0–5.5) months, TTP was 4.4 (3.0–5.5) months, BeFS was 8.6 (6.9–11.9) months, and BMF was 5.8 (3.3–8.6) months (Fig. 1). Among the 110 patients studied, 50 (45 %) died, 85 progressed (77 %), and 24 (22 %) suffered a skeletal-related event. Only 92 of the 110 patients had a sufficiently long enough follow-up time to evaluate BMF and among these, 32 (35 %) developed BMF.
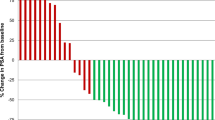
A significant association between RaTot and OS, PFS, BeFS, and BMF was observed for the mCRPC patients in this study (Table 3), independently and when adjusting for other measures (multivariable analysis). An increase in the number of 223Ra cycles reduced the risk of each outcome. In addition, more 223Ra cycles delivered were significantly associated with a reduction in pain scores (p = 0.041) (Fig. 2) and ALP levels (p < 0.0001) (Fig. 3).
Tolerability of 223Ra
Prior to their first 223Ra cycle, 13 patients had Hb levels below 10.0 g/dl (6.6–9.8 g/dl). None of these patients received erythropoietin-stimulating agents 4 weeks prior to 223Ra. The evaluation of hematologic toxicity was possible in 92 patients. The mean and median times to nadir were 3.3 weeks, with a maximum of 6.5 weeks.
During 223Ra, hematologic toxicity was grade 3 in 1.9 % of patients and 0 % had grade 4 toxicity. However, after 223Ra, BMF occurred in 32/92 patients (11 due to grade 4 toxicity and 18 due to grade 3 toxicity). Grade 4 thrombocytopenia occurred in ten patients (11 %) and grade 3 thrombocytopenia in ten patients (11 %). BMF was clinically attributed to disease progression in nine (10 %) patients that developed G3/G4 anemia with only G1/G2 thrombocytopenia. BMF was clinically attributed to 223Ra in four (4 %) patients that had G3/G4 thrombocytopenia with only G1/2 anemia. Finally, BMF may have been induced by 223Ra in an additional 16 patients (17 %) that developed G3/G4 anemia associated with G3/G4 thrombocytopenia.
Of the 32 patients who developed BMF, 5 received concurrent chemotherapy during their 223Ra cycles, including cyclophosphamide (n = 6), cabazitaxel (n = 1), mitoxantrone (n = 1), and paclitaxel (n = 1). However, there was no statistically significant increased risk of BMF in patients treated with concomitant 223Ra and chemotherapy compared to like those treated with 223Ra alone (p = 0.71).
Of the patients who developed BMF, three patients had EBRT concurrent to 223Ra and two had EBRT after 223Ra; the association between BMF development and the use of EBRT was significant (p = 0.009) and an independent predictor (p = 0.013) (Table 4).
The development of BMF in relation to 223Ra therapy was in itself a predictor of survival. The median OS for the 60 patients who did not develop BMF was not reached [18 of the 60 (30 %) died], while the median OS (95 % CI) for the 32 patients that did develop BMF was 6.97 months (5.68–8.21), where 28 of the 32 (88 %) patients died.
Clinical and laboratory parameters and time-to-event outcome measures
Based on imaging, 55 (50 %) patients were categorized as having high skeletal tumor burden, 35 (32 %) intermediate skeletal tumor burden, and 20 (18 %) low skeletal tumor burden. Nodal metastases at baseline were noted in 26 (24 %) patients and were located in the abdomen and pelvis in 19 patients and in the thorax and abdomen/pelvis in 7 patients. Visceral metastases at baseline were present in 13 (12 %) patients and these lesions were located in the brain (n = 1), liver (n = 7), and lungs (n = 5). In all cases, visceral metastases were previously treated and felt to be quiescent. In addition, four patients had prior history of secondary cancer (one follicular lymphoma, one renal cell carcinoma, and two bladder cancers).
Tables 3 and 4 describe the outcome measures in relation to the clinical and laboratory parameters. Pain score above 2 prior to 223Ra was significantly associated with a higher risk of death, progression, skeletal-related events, and development of BMF (p ≤ 0.001). Baseline severe skeletal pain was the only variable that remained significantly associated with increased risk of a skeletal-related events, when controlling for other measures (multivariable analysis) (p = 0.042).
A decline in ECOG status prior to 223Ra significantly increased the risk of death, progression, of a skeletal-related event, and of developing BMF (p ≤ 0.008). Moreover, there was a threefold increase in the risk of progression after 223Ra treatment with an ECOG > 2 [hazard ratio (HR) = 3.79; 95 % CI 2.39–5.99; p value < 0.0001] (Fig. 4). However, on multivariable analysis the ECOG status was not significantly associated with any of the outcome measures.
Trend in ECOG score from the 1st to the 6th 223Ra cycles. Although there is not a significant overall change in the patient’s ECOG status throughout the 223Ra therapy, a slight increase in ECOG score occurred at the 3rd 223Ra cycle at which time the patients progressed. Afterwards, the ECOG score decreases (patient status improved)
ALP ≥ 146 UI/l prior to beginning the 223Ra cycles was significantly (p ≤ 0.010) associated with a higher risk of death, progression, skeletal-related events, and developing BMF. When considering other measures (multivariable analysis) ALP ≥ 146 UI/l was not associated with any of the outcome measures.
An initial PSA > 10 ng/ml doubled the risk of progression (p = 0.011) but this significant association was not maintained with multivariate analysis. Additionally, the PSADT from first 223Ra cycle to last 223Ra cycle was not associated with OS, PFS, BMF, and BeFS. On the other hand, PSADT calculated at two consecutive 223Ra cycles was significantly associated with OS, PFS, TTP, and BeFS. PSADT of less than 3 months increased the risk of each outcome by at least fivefold compared with PSADT ≥ 3 months (p ≤ 0.006) (Fig. 5).
Trend in PSADT (in months) from the 1st to the 6th 223Ra cycles. Between the 1st and 2nd 223Ra cycles, the mean PSADT is 3.78 months. Throughout therapy, as the patients present signs of disease progression at the 3rd 223Ra cycle, it is clearly noted that the PSADT rate increases (mean = 2.2 months from the 2nd to 3rd dose and mean = 0.55 months from the 3rd to 4th dose). Afterwards, the PSADT rate reduces (mean = 2.35 months between the 4th and 5th dose)
A baseline Hb level below 10 g/dl was associated with a fourfold increase in the risk of developing BMF (p < 0.001) although this association did not persist when adjusted for other measures (multivariable analysis).
Treatments performed prior to, during, and after 223Ra cycles
Tables 3 and 4 describe the outcome measures in relation to the treatment regimens, and Table 5 describes the types of treatments performed prior to, during, and after 223Ra. All patients were receiving prednisolone, bisphosphonates, and luteinizing hormone-releasing hormone (LHRH) analogue therapy.
Prior to 223Ra cycles, 55 patients had received secondary hormone therapy, 56 patients had undergone chemotherapy, and 16 patients were treated with EBRT. The median time to initiate a secondary hormone therapy prior to the first 223Ra cycle was 9.3 weeks (0–36.3 weeks), while the median time to end chemotherapy prior to the first 223Ra cycle was 6.7 weeks (0–165.7 weeks). There was no significant difference in OS, PFS, or BeFS between patients receiving or not receiving chemotherapy prior to 223Ra, nor was there a difference in the risk of developing BMF.
The median time between completion of EBRT and initiation of 223Ra was 9.2 weeks (1.9–70.1 weeks). The use of EBRT prior to 223Ra was not associated with any improvement in OS, PFS, or BeFs and was not associated with increased risk of BMF.
At the end of 223Ra therapy, 49 patients either began or continued a secondary hormone therapy regimen, with a median time to begin treatment of 13.9 weeks from the first 223Ra cycle. There was a significant benefit in the use of abiraterone concomitant to 223Ra in terms of OS, PFS, and BeFs (univariable: p < 0.002 and multivariable: p < 0.044). The use of abiraterone with 223Ra reduced the risk of death and of a skeletal-related event by 77 % and the risk of progression by 68 %. On the other hand, the use of enzalutamide concomitant to 223Ra did not improve outcome in these patients.
Chemotherapy was administered to 13 (12 %) patients during 223Ra treatments and to 27 (25 %) patients after completion of 223Ra treatments. The median time to begin chemotherapy after initiation of the first 223Ra cycle was 15.1 weeks (0–57.3 weeks). EBRT was performed concurrently with 223Ra in 13 (12 %) patients, with a median time to begin EBRT of 16.4 weeks (0.1–29.3 weeks).
Discussion
223Ra dichloride is approved for clinical use in patients with CRPC and symptomatic skeletal metastases based on an improvement in OS compared to patients receiving placebo [2]. However, experience suggests that not all patients receive the same level of benefit from 223Ra. One challenge has been to identify factors that may predict response to radium and to identify patients in whom radium may not control their disease. Additionally, there is debate over the timing of radium administration in the course of disease, whether to administer early on or to delay until other options have been exhausted.
In this study, we reviewed our extensive clinical experience with 223Ra in patients with prostate carcinoma. These patients represented a broad spectrum of demographics, including age, disease burden, laboratory values, and prior and concurrent therapies. We retrospectively assessed these clinical parameters for their association with outcome measures including OS, PFS, BeFS, and development of BMF.
Overall, we found that 223Ra had a clear benefit in the treatment of mCRPC patients. There was a significant correlation between the number of radium doses delivered and better outcome. Patients who completed the planned six-cycle 223Ra therapy had a reduced risk of death (−44 %), progression (−33 %), skeletal-related event (−38 %), and development of BMF (−30 %) compared to patients who did not receive all six doses. We conducted a subgroup analysis of patients that did not complete all six cycles of 223Ra due to progression and were switched to chemotherapy with those patients that, despite progression, completed all six cycles of 223Ra. The median OS of the second group (15.7 months) was significantly longer than the first group (7.2 months; p < 0.0001). Even after excluding those patients who discontinued the 223Ra cycles because of unrecoverable hematologic toxicity, 223Ra was still beneficial (OS: HR = 0.44; 95 % CI 0.33–0.59; p < 0.0001). Notably, patients who discontinued 223Ra because of progression (either skeletal or extraskeletal) and were switched to another therapy had worse outcomes compared to patients who continued with 223Ra despite progression.
Although our patients had a median OS time of 12 months, shorter than the phase III placebo-controlled trial [2] (median OS = 14 months), our patient population is somewhat different from that in the trial. At initial diagnosis, prior to the first 223Ra cycle, 82 % of our patients had skeletal tumor burden classified as high or intermediate. Additionally, 12 % had visceral metastases and 24 % had nodal metastases. Even despite these factors, we confirm a benefit to 223Ra therapy in these patients with more advanced disease (Table 6).
Similar to other reports that have identified skeletal parameters as prognostic markers of survival in mCRPC patients [4], we found that the presence of bone pain, ALP ≥ 146 UI/l, and a poor ECOG status were predictive of OS, PFS, BeFS, and BMF. In addition, the presence of bone pain independently predicted the risk of a skeletal-related event in these patients.
In the majority of the patients there was a significant reduction in pain and ALP levels and improvement in the ECOG status throughout the 223Ra cycles (Fig. 6), as has been previously reported [7]. However, increased pain during 223Ra occurred in 14 % of the patients due to a flare phenomenon, especially between the first and second cycles. Because of the intensity of the flare phenomenon, 5 % of the patients had to discontinue 223Ra or had to undergo EBRT to control pain. Although the flare phenomenon has been described in prior studies with 223Ra in CRPC patients, none have described the rate of discontinuation of 223Ra cycles due to the intensity of the pain [8, 9]. The patients that developed a flare response had a remarkable symptomatic improvement in the subsequent cycles. Comparing those six patients with the rest of the sample, there was no significant difference in OS, although patients with a flare response had shorter median OS (median: flare = 8.3 months, no flare = 11.7 months; p = 0.27).
Example of a good response to 223Ra cycles in an 84-year-old patient diagnosed 3 years ago with a stage IV mCRPC (Gleason 9 and bone metastases). Despite secondary hormonal therapy and narcotic pain medication, he was losing weight, his pain was increasing, ECOG status was declining, and the patient’s PSA and ALP levels were steadily rising. a The whole-body 18F-fluoride PET/CT prior to the first 223Ra cycle demonstrated multiple osteoblastic bone metastases, especially in the lumbar spine and pelvis. After the 1st 223Ra cycle and prior to the 2nd cycle, although the patient had a flare response, he gained weight. Between the 2nd and 3rd cycles, his ECOG status improved (from 1 to 0). b The patient’s PSA levels declined from 8.4 ng/ml at the 1st 223Ra cycle to 0.0 ng/ml after the 4th 223Ra cycle and was maintained at 0 thereafter. c The patient’s ALP levels declined from 268 IU/l at the 1st 223Ra cycle to 70 IU/l after the 4th 223Ra cycle. d An interim whole-body 18F-fluoride PET/CT scan (performed immediately prior to the 4th 223Ra cycle) demonstrated marked improvement of the bone metastases, with reduction of uptake
Surprisingly, there was a clear OS and PFS benefit of the concomitant use of 223Ra with abiraterone. In our population, patients receiving abiraterone plus 223Ra had a 77 % reduction in the risk of death, 88 % reduction in the risk of a skeletal-related event, and a 68 % reduction in the risk of progression. Phase III trials found a survival benefit of the abiraterone arm when evaluating abiraterone vs placebo (14.8 vs 10.9 months) and especially in patients progressing after docetaxel (15.8 vs 11.2 months) [10–12]. A synergistic interaction between abiraterone and EBRT has been described [13], and the same may hold true for the concomitant use of abiraterone and 223Ra.
Despite prior studies demonstrating a survival benefit of treating mCRPC patients with enzalutamide [14], a recent comparison of the phase II trials evaluating enzalutamide and abiraterone found no significant difference in OS among these two secondary hormone therapies [15]. In our patient population, enzalutamide concomitant to 223Ra did not demonstrate a significant OS or PFS advantage.
One might argue that the comparative benefit of abiraterone vs enzalutamide in our patient population may be due to a difference in patient selection as patients that were on abiraterone might have had a lower burden of disease than those on enzalutamide. However, in our study, mCRPC patients with initial ECOG status 2 and 3 were more prevalent in the abiraterone group than the enzalutamide group (14 vs 7 %, respectively). Similarly, more mCRPC patients underwent chemotherapy prior to 223Ra in the abiraterone group than in the enzalutamide group (51 vs 46 %, respectively). Therefore, patients that had abiraterone plus 223Ra had, in general, at least a similar (if not higher) burden of disease.
223Ra was well tolerated with minimal hematologic toxicity during cycles, with only 2 % of patients experiencing grade 3 toxicity and none grade 4 toxicity. However, BMF occurred in a significant number of patients (35 %), despite the fact that 223Ra was beneficial even in patients with a high tumor burden (as 80 % of our patients had extensive disease). BMF was most likely induced by 223Ra in 4 % of the patients and may have been induced by 223Ra in an additional 17 %. Interruptions of 223Ra due to hematologic toxicity occurred in 15 % of our patient population. These results are higher than those reported in the literature [16]. Anemia is a common outcome in CRPC patients; however, abnormal platelet and white blood cell counts are rare [17]. Consequently, thrombocytopenia was clearly an effect of radiation as PLT have the highest turnover and because none of the patients were submitted to chemotherapy regimens (such as carboplatin) that cause major thrombocytopenia. Although Hb < 10 g/dl has been described as predictive of BMF, among the 20 patients that developed thrombocytopenia only 2 had prior anemia (both levels were 9.8 g/dl), while among the 9 patients with BMF due to anemia (without thrombocytopenia) 5 had initial Hb levels below 10 g/dl, 3 of them with very low values (6.6, 7.5, and 8.1 g/dl). There was no association between the use of chemotherapy and the development of BMF. On the other hand, there was a significant association between developing BMF with the concomitant use of 223Ra and EBRT. None of the clinical and laboratory parameters were independent predictors of the risk of developing BMF. To that effect, imaging biomarkers with 18F-fluoride PET/CT may be useful to predict this outcome [18].
There are limitations to this study, as this was not a prospective randomized trial but rather an observational study based on clinical experience. As such, the 110 patients we examined are a heterogeneous group from actual clinical practice. The majority had a high burden of disease, and not all patients completed the full six cycles of 223Ra, either due to clinical intolerance or medical decision to discontinue. Additionally, the concomitant drug regimens were heterogeneous. When the patients progressed during 223Ra, it was the oncologist’s decision to discontinue 223Ra and implement chemotherapy (or secondary hormone therapy) or to continue 233Ra with the addition of other drugs (either chemotherapy or secondary hormone therapy).
Overall, the heterogeneity of the population provides a broad perspective on the use of 223Ra in routine clinical practice and provides interesting observations and suggestions of mechanisms and outcomes. In particular, the improved outcomes with continuation of 223Ra despite clinical or imaging evidence of progression and with the concurrent use of 223Ra and abiraterone are intriguing and bear further investigation in a prospective trial.
Conclusion
This study describes new aspects of 223Ra therapy in mCRPC patients. As this study was conducted outside a regulatory trial, many factors that might influence 223Ra therapy were identified. Unlike previous trials, the patient population was composed of individuals with extensive bone disease and also some that had visceral and/or nodal metastases.
Our patients were able to tolerate chemotherapy and secondary hormonal therapy concomitant to 223Ra. Therefore, even in patients with visceral metastases 223Ra can perhaps be considered alongside with chemotherapy, as there is a clear benefit in terms of OS, PFS, and BeFS. For further definition of the safety and tolerability of such an approach, prospective trials will be needed. Additionally, patients who progress during 223Ra (developing visceral, nodal, or bone metastases) may benefit from the combination of 223Ra and another treatment modality.
Although BMF may occur after 223Ra, the median OS for the patients who did not develop BMF was not even reached despite having extensive skeletal metastases. The chemotherapy regimens used concurrent to 223Ra in our study group were not associated with an increased risk of BMF. On the other hand, there was an increased risk of developing BMF with the simultaneous use of EBRT. The consequences of the use of EBRT during 223Ra have not yet been described and warrant further study. Since ALP levels did not predict BMF, the determination of ALP levels prior to 223Ra does not seem a helpful guide to determine the possible risk of developing BMF.
Finally, abiraterone used concurrently with 223Ra seemed to have a positive effect in our patients. There is an ongoing randomized trial (NCT02043678) evaluating the use of abiraterone and 223Ra, which may confirm our initial findings.
References
Hoskin P, Sartor O, O’Sullivan JM, Johannessen DC, Helle SI, Logue J, et al. Efficacy and safety of radium-223 dichloride in patients with castration-resistant prostate cancer and symptomatic bone metastases, with or without previous docetaxel use: a prespecified subgroup analysis from the randomised, double-blind, phase 3 ALSYMPCA trial. Lancet Oncol 2014;15:1397–406. doi:10.1016/s1470-2045(14)70474-7.
Parker C, Nilsson S, Heinrich D, Helle SI, O’Sullivan JM, Fosså SD, et al. Alpha emitter radium-223 and survival in metastatic prostate cancer. N Engl J Med 2013;369:213–23. doi:10.1056/NEJMoa1213755.
Nilsson S, Franzén L, Parker C, Tyrrell C, Blom R, Tennvall J, et al. Two-year survival follow-up of the randomized, double-blind, placebo-controlled phase II study of radium-223 chloride in patients with castration-resistant prostate cancer and bone metastases. Clin Genitourin Cancer 2013;11:20–6. doi:10.1016/j.clgc.2012.07.002.
Fizazi K, Massard C, Smith M, Rader M, Brown J, Milecki P, et al. Bone-related parameters are the main prognostic factors for overall survival in men with bone metastases from castration-resistant prostate cancer. Eur Urol 2015;68:42–50. doi:10.1016/j.eururo.2014.10.001.
Jadvar H, Challa S, Quinn DI, Conti PS. One-year postapproval clinical experience with radium-223 dichloride in patients with metastatic castrate-resistant prostate cancer. Cancer Biother Radiopharm 2015;30:195–9. doi:10.1089/cbr.2014.1802.
Kelloff GJ, Coffey DS, Chabner BA, Dicker AP, Guyton KZ, Nisen PD, et al. Prostate-specific antigen doubling time as a surrogate marker for evaluation of oncologic drugs to treat prostate cancer. Clin Cancer Res 2004;10:3927–33. doi:10.1158/1078-0432.ccr-03-0788.
Humm JL, Sartor O, Parker C, Bruland OS, Macklis R. Radium-223 in the treatment of osteoblastic metastases: a critical clinical review. Int J Radiat Oncol Biol Phys 2015;91:898–906. doi:10.1016/j.ijrobp.2014.12.061.
Den RB, Doyle LA, Knudsen KE. Practical guide to the use of radium 223 dichloride. Can J Urol 2014;21:70–6.
Nilsson S, Larsen RH, Fosså SD, Balteskard L, Borch KW, Westlin JE, et al. First clinical experience with alpha-emitting radium-223 in the treatment of skeletal metastases. Clin Cancer Res 2005;11:4451–9. doi:10.1158/1078-0432.ccr-04-2244.
de Bono JS, Logothetis CJ, Molina A, Fizazi K, North S, Chu L, et al. Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med 2011;364:1995–2005. doi:10.1056/NEJMoa1014618.
Beckett RD, Rodeffer KM, Snodgrass R. Abiraterone for the treatment of metastatic castrate-resistant prostate cancer. Ann Pharmacother 2012;46:1016–24. doi:10.1345/aph.1Q758.
Fizazi K, Scher HI, Molina A, Logothetis CJ, Chi KN, Jones RJ, et al. Abiraterone acetate for treatment of metastatic castration-resistant prostate cancer: final overall survival analysis of the COU-AA-301 randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol 2012;13:983–92. doi:10.1016/s1470-2045(12)70379-0.
Hingorani M, Dixit S, Pugazhenthi P, Hawkyard S, Robertson A, Khafagy R. Can palliative radiotherapy influence prostate-specific antigen response in patients with castrate-resistant prostate cancer treated with systemic therapy (chemotherapy or abiraterone)?-a report of three cases. Cancer Biol Med 2015;12:60–3. doi:10.7497/j.issn.2095-3941.2014.0025.
Graff JN, Gordon MJ, Beer TM. Safety and effectiveness of enzalutamide in men with metastatic, castration-resistant prostate cancer. Expert Opin Pharmacother 2015;16:749–54. doi:10.1517/14656566.2015.1016911.
Tan PS, Haaland B, Montero AJ, Kyriakopoulos CE, Lopes G. Hormonal therapeutics enzalutamide and abiraterone acetate in the treatment of metastatic castration-resistant prostate cancer (mCRPC) post-docetaxel-an indirect comparison. Clin Med Insights Oncol 2014;8:29–36. doi:10.4137/cmo.s13671.
Yeku O, Slovin SF. Metabolism and pharmacokinetics of radium-223 in prostate cancer. Expert Opin Drug Metab Toxicol 2015;11:843–9. doi:10.1517/17425255.2015.1021332.
Geenen RW, Delaere KP, van Wersch JW. Haematological variables in prostatic carcinoma patients. Acta Urol Belg 1996;64:21–6.
Etchebehere E, Araujo JC, Milton D, Fox P, Swanston N, Macapinlac H, et al. Skeletal tumor burden on baseline 18F-fluoride PET/CT to predict bone marrow failure after radium-223. J Clin Oncol 2015;33:S11012.
Research funding
This work is supported in part by the James E. Anderson Distinguished Professorship Endowment, by the Cancer Center Support Grant (NCI Grant P30 CA016672), and Fundação Amparo à Pesquisa da Universidade de São Paulo (FAPESP 2014/03317-8).
Compliance with ethical standards
ᅟ
Authors’ disclosures of potential conflicts of interest
All authors declare that they have no conflict of interest. The authors declare no financial (or other) conflict of interest relating to employment or leadership position, consultant or advisory, stock ownership, honoraria, expert testimony, patents, royalties, licenses, or other remuneration.
Ethical approval
This study was approved by the Institutional Review Board (PA14-0848). Waivers of Informed consent and authorization were granted for the retrospective analysis of the imaging data. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Etchebehere, E.C., Milton, D.R., Araujo, J.C. et al. Factors affecting 223Ra therapy: clinical experience after 532 cycles from a single institution. Eur J Nucl Med Mol Imaging 43, 8–20 (2016). https://doi.org/10.1007/s00259-015-3185-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-015-3185-4